Plantar fasciitis is one of the most common orthopaedic complaints and so I thought it was important to explore the potential treatments for an injury that is prevalent amongst distance runners and athletes who spend long periods on their feet...
What is the plantar fascia?
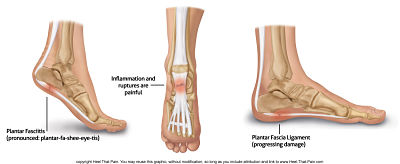
When referring to the plantar fascia, most people are referencing the thick web-like ligament (bone to bone) which anchors at the heel and fans out to the metatarsal heads at the front of the foot.
This essential part of the foot structure acts as a shock absorber, helps us to spread load through the foot structure, enables us to maintain balance, holds the shape of our arch, and is a vital component to most movement involving feet.
Exploring the plantar fascia
Kick your footwear off and place your feet flat on the floor.
Now, keeping your feet flat on the floor, press all of your toes as hard into the ground as possible. The harder you press, the higher your arch will raise, and your toes will curl in towards the foot, and squeeze them as tight closed in a foot fist as you can.
You may notice that this requires your calves to contract, for some considerably more than others, and we will talk about this further in a bit.
To enable the movement to happen, the plantar fascia was required to interact with the other controlling structures by contracting in length and holding strength.
If we now do the complete opposite - start with a flat foot on the floor and raise all of the toes in the air as high as possible. You may feel that it's the front and side of the lower leg which must contract to support this function, and that we can feel activity through the outside of the ankle.
To assist and enable this function, the plantar fascia has had to release under control and extend in length, allowing the range of motion through the toes.
As a final test, if we stand with our feet flat on the floor and raise up in a ‘calf raise’, keeping the balls of the feet and all the toes pressed into the floor, we can feel that the plantar fascia is required to maintain the foot shape through the motion.
If we then lower and raise in a controlled manner, we can feel that the foot is retaining shape whilst the calf, ankle, and other structures manage the movement to pivot the balls of the feet. Here the fascia is acting as a ‘retainer’ to hold structure and inter-connect the movement.
Diagnosis (and misdiagnosis) of ‘plantar fasciitis’
A few years ago, I was visiting a running group in the capacity of coach mentor when, during the stretch component of a warm-up, I witnessed a member of the group mention some foot pain they were experiencing in the sole of their foot.
Suddenly 'Dr Google' was in surgery, “that’s classic plantar fasciitis, you need to roll your foot every day on a golf ball”. Not wanting to be rude, but also not wanting to leave anything unmentioned I said; “wow, that’s a really quick diagnosis, how did you rule out fat pad atrophy, osteomyelitis, and tarsal tunnel syndrome?”.
Personally, I think plantar fasciitis is grossly misdiagnosed, and can quite often go hand-in-hand with additional complexes such as a heel spur. Other conditions to take into consideration in diagnosis of base foot pain include:
Neurologic: Tarsal tunnel syndrome Entrapment neuropathy Peripheral neuropathy Lumbar radiculopathy |
Arthritic: Rheumatoid arthritis Ankylosing spondylitis Reiter's disease Inflammatory arthropathies |
Skeletal: Calcaneal stress fracture Bone contusion Osteomyelitis Paget's disease Calcaneal apophysitis |
Other: Vascular insufficiency Neoplasm Enthesopathies Fat-pad atrophy Achilles tendonitis |
Due to its given suffix ‘itis’, plantar fasciitis is implied to be a condition with inflammation. However, there's plenty of studies which suggest that the condition is one more of atrophy/degeneration than inflammation, thus would be better named plantar fasciosis or fasciopathy.
Certainly, pretty much all of the cases I've witnessed with medically diagnosed plantar fasciitis have not been obvious through visible swelling or inflammation.
I like the safety of sitting on the fence but on this one I’m leaning heavily over the fasciosis garden. Suffice to say, you may not have visible swelling in the event you do have plantar fasciitis/osis.
Symptoms of plantar fasciitis
Plantar fasciitis pain presents mainly directly underneath the heel, or towards the bottom mid-foot area. The pain typically develops gradually over time and can begin as quite a dull pain, developing into a much sharper debilitating pain.
In some cases, the condition can present with hotness and even a ‘burning’ sensation on the bottom of the foot extending from the heel.
Unlike many conditions, plantar fasciitis can actually seem to rescind with activity and return with a vengeance afterwards. For this reason, it can be severe when waking in the morning and incredibly painful taking the first steps of the day, easing as movement is promoted.
Inactivity seems to promote a stiffness in the heel and prolonged activity can flare the pain to leave several days of aggravation. Plantar fasciitis can leave the foot tender to touch and also affect motor control, such as balance and coordination.
Treatment of plantar fasciitis
At first:
In the first instance, suspected plantar fasciitis should be treated as a ligament injury. So, follow the rules:
- Rest
- Ice
- Compression
- Elevation
- Manipulation
- Exercise
One of my tips for remedial relief is to keep a small bottle of water in the freezer, so when the injury flare ups you can roll the foot and heel over the icy cold bottle.
As we explored earlier, the plantar fascia can be affected even by having a tight calf or Achilles tendon, and so exercises should include mobility, subtlety, and strength from the lower leg right the way through the foot structure.
Band restrained flexes of the foot in all directions will help with mobility and strength, especially if they're done with toes fully contracted and also fully extended.
Short to medium term:
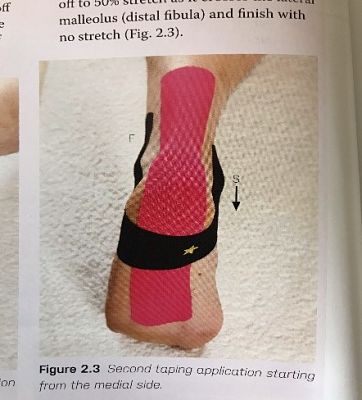
In his book ‘Kinesiology taping for injury prevention and medical conditions’, John Gibbons cites the work by Tsai et al. (2010) which concluded that patients that received kinesiology taping continuously for a week elicited greater improvements than those who underwent only physical therapy.
I’ve used John’s taping method to good effect myself and can confirm that the clients have all expressed positive effect. In some people, this may be enough to allow the healing process to complete, while it will act as a remedial relief in other longer-term and more serious cases.
Medium to long term:
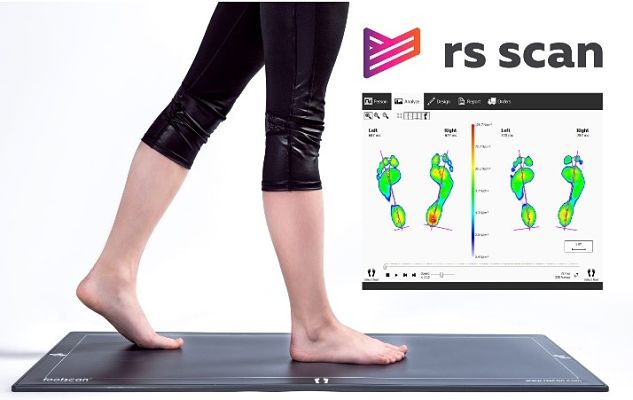
In the medium to long-term, people who periodically or continually suffer with plantar fasciitis could benefit from custom orthotics.
As a Specialist Gait and Motion Clinician, I personally use the 1-metre RS Footscan for analysis which is then projected through to Phits Orthotics who bespoke 3-D print the left and right foot orthotics separately.
We're hoping that this type of cutting edge technology will become more widely issued and keep progressing as it really does make a difference.
By assessing each foot individually and utilising the 3-D print technology, we're able to adapt the orthotics far more than a stock set of foam shoe inserts. Just recently I was able to produce a custom pair of orthotics for a client with a previously operated on Morton’s Neuroma in her left foot and plantar fasciitis in the right.
Long term:
Long-term and aggressively persistent plantar fasciitis may require medical intervention.
Developments here have been positive in therapies such as extracorporeal shockwave therapy (ESWT) for refractory plantar fasciitis.
Quite often a corticosteroid injection is put forwards as a potential form of treatment, and in extreme cases surgery may be discussed as an option.
On the steroid injection front, if it was me personally, I would read all of the studies and exhaust all other avenues before taking this option, given that the corticosteroid injections have a clinically recognised risk of heel fat pad atrophy or plantar fascia rupture – it’s a low risk but it’s there.
For more information, visit The Woodland Clinic website or contact Ben Cox Physiology and Coaching directly.
