A study published in 2019 investigated how taking part in gruelling endurance challenges like the Tour de France, an IRONMAN and Race Across the USA affects the human body and found that one of the toughest challenges you can participate in is carrying a baby in your womb for 9 months.
What does that mean for expectant mums who want to train whilst pregnant? Is it safe? How much is too much? Let’s take a look...
Comparing pregnancy with endurance events
The study focused on the Basal Metabolic Rate (BMR) - or resting energy expenditure - of participants during certain activities and found that we can sustain a maximum of 2.5x our BMR, which is the ‘ceiling’ of human endurance.
Athletes completing the gruelling ‘Race Across The USA’ levelled out at 2.4 times their BMR toward the end of the 140-day race. Pregnancy sat only slightly lower than this at 2.2 times BMR, but let’s not forget that pregnant women maintain this rate for 9 entire months with very little time for recovery afterwards, what with a new-born baby to look after!
You could argue that pregnancy is the longest, toughest endurance event there is. So, you’d understand if mums-to-be decided not to train whilst pregnant. But many expectant mothers do train and if you’re considering doing the same but are unsure, we’ve taken a look at what the guidance and science out there has to say about how to do so safely...
The ‘official’ guidelines for training during pregnancy
Research may have shown that exercising during pregnancy is safe - and that it benefits both mum and baby - but many women are still unsure about how to manage their training load because of a lack of clear guidance about how much is too much.
Both the UK and US governments’ guidelines suggest that pregnant women should aim to complete at least 150 minutes of moderate intensity activity every week. But, that’s the same advice given to the non-pregnant population, so it’s no wonder that many women are left feeling uncertain about how to approach exercise during their pregnancy!

What does the scientific literature say about training during pregnancy?
Fitting with the above ‘official’ guidelines, a number of studies have shown that exercise of low-to-moderate intensity is safe during an uncomplicated pregnancy (see here, here and here). And a 2021 study showed that there are positive outcomes associated with exercise for both expectant mothers and their fetuses.
What’s becoming increasingly common is that women who are already physically active at a high athletic level pre‐conception want to continue training vigorously during pregnancy, but the consensus around how achievable that is remains less clear.
Most top athletes understand that gaining fitness during pregnancy is an unrealistic goal but what they do want is reassurance that they can undertake activity which (to the best of their ability) maintains fitness.
A study conducted at the University of Oslo in 2005 set out to tackle two areas of concern:
- whether vigorous training in pregnant athletes could be conducted without a risk to mother and foetus health
- to define a safe training regime for the maintenance of fitness in top‐level female athletes during pregnancy
Recruiters gave 41 top competitive pregnant athletes the choice to participate either in a high‐volume exercise group (~8.5 hours/week, 6 days/week), a medium‐volume exercise group (~6 hours/week, 4 days/weeks) or a non‐exercising control group (of which none were willing to be in!).
During their pregnancies, the exercise programs the women underwent consisted of three parts: muscle strength training (which targeted all the major muscle groups), aerobic interval training and appropriate aerobic endurance training (cycling, fast walking or cross-country skiing).
The research group demonstrated that vigorous exercise during pregnancy by women who are well trained pre‐conception could be performed without detriment to the course of pregnancy, labour or the foetus, and that it benefited the mother. The general conclusion was also that high fitness levels could be maintained during pregnancy when appropriately strenuous training is continued.
So, how does this look in practice during a nine-month pregnancy?
A case study which looked at how Marit Bjørgen (one of the most successful Winter Olympians of all time) trained whilst pregnant provides an interesting example.
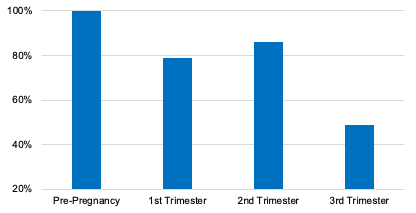
The study found Marit’s training volumes changed as she moved through the three trimesters of her pregnancy.
- First trimester = 79% of pre-pregnancy training volume
- Second trimester = 86% of pre-pregnancy training volume
- Third trimester = 49% of pre-pregnancy training volume
Other observations:
- The amount of high intensity training reduced significantly, and wasn’t performed after week 5 of pregnancy
- Strength training was performed throughout the entire pregnancy, but with a clear reduction in volume during the third trimester
- The strength training was gradually modified to involve more upper body exercises and less focus on abdominal muscles and squat movements
How should you train during pregnancy?
Beyond the generic “150 minutes per week” guidelines, there aren’t any hard and fast rules on how much training is the right amount for you. But, here are 7 things to consider when planning your training during pregnancy...
- Shift your focus towards maintenance rather than improvement. Tracking your training in minutes rather than miles and in terms of effort, rather than pace, can really help you to adapt to this new way of training. Pro triathlete Mary Robbins told us, “I’ve found a lot of peace in letting go of pace, metrics, and power numbers, and just training for the joy of it during pregnancy.”
- Keep exercise intensity below 90% of maximum heart rate or VO2 max. You may find you need to reduce the intensity further throughout your pregnancy which is completely normal – listen to your body
- Think about your nutrition and hydration needs as a pregnant woman AND an athlete. It’s important to ensure you’re taking on enough to fuel training, recovery and pregnancy
- Keep up the strength training. Strength will be important in supporting your bump, adapting to your new centre of gravity, and help to lower your risk of injury. Be careful to avoid the supine position (lying on your back) as this can compress the inferior vena cava (a large vein responsible for returning blood back to the heart) which could lead to decreased blood flow to the foetus. As an alternative, strength exercises can be done in sitting, standing or side-lying positions.
- Get the all clear from your doctor to make sure there are no medical reasons why you should avoid certain workouts, movements or higher intensities of exercise
- Keep in mind the warning signs that suggest you need to stop exercising. These include increased shortness of breath, headaches, dizziness, chest pain and vaginal bleeding
- Avoid exercises that could cause overheating, energy deficiency, dehydration, falling, or contact / collision (e.g. ice hockey, martial arts, horse riding, gymnastics, scuba diving and skiing)
It’s also worth getting advice from your coach, or finding a coach that specialises in pregnancy and post-natal training advice, if you’re seeking help with personalising your training to how you feel during your pregnancy.

Pro athletes and the sponsorship conundrum
In the pro sphere, Serena Williams and Paula Radcliffe are two famous examples of women who continued to train and even compete during pregnancy. Serena won the 2017 Australian Open without dropping a single set despite being in her first trimester during the tournament. And Paula reportedly trained twice a day for much of her pregnancy and won the 2007 New York Marathon just 10 months after giving birth.
These achievements are rightly heralded as remarkable feats of endurance, although concerns have been raised that some pro athletes continue to train and compete during pregnancy for fear of repercussions from their sponsors.
World Championships medallist Alysia Montaño, Olympian Kara Goucher, and American track legend Allyson Felix told The New York Times that Nike penalised them for being pregnant by stopping payments while they were unable to compete during pregnancy.
In a hugely positive step in the right direction, the Professional Triathletes Organisation (PTO) stated that “no one should ever be penalised for getting pregnant” and launched a maternity leave policy that allows women to take 15 months off from the sport while still retaining an income. Their PTO rankings will also remain fixed during that period.
One-size-definitely-doesn’t-fit-all
When it comes to athletes and pregnancy, it’s clear that there’s still work and research to be done around education for athletes, sponsors and coaches. As with so much of sports science, there isn’t a ‘one size fits all’ approach to training during pregnancy.
We spoke to pro triathletes with PH in their bottles to find out how they adjusted their training volume during pregnancy and their experiences differed significantly.
Pregnant women should seek to maintain movement during pregnancy and what that looks like is different for everyone, so your “maintenance” should be relative to your pre-pregnancy activity levels.
If you weren’t a marathon runner before you fell pregnant, now’s probably not the time to test out if you’re the next Paula Radcliffe with 4-5 run sessions a week! Whereas if you were training ~20 hours a week before you fell pregnant, you may well be able to continue to train a fair bit whilst managing your expectations as your body goes through a raft of changes.
